Does Cholesterol Aggravate Symptoms of Varicose Veins?
Varicose veins are swollen, enlarged veins that usually appear in the legs and feet due to poor circulation. While genetics, age, and lifestyle factors like prolonged standing or sitting are commonly known causes, there’s growing interest in how cholesterol and cardiovascular health may impact the development and symptoms of varicose veins. High cholesterol is a risk factor for heart disease, but does it also play a role in worsening varicose vein symptoms?
This article will explore the relationship between cholesterol and varicose veins, examine whether elevated cholesterol levels can aggravate symptoms, and offer practical advice on managing both conditions.
Understanding Varicose Veins and Cholesterol
What Are Varicose Veins?
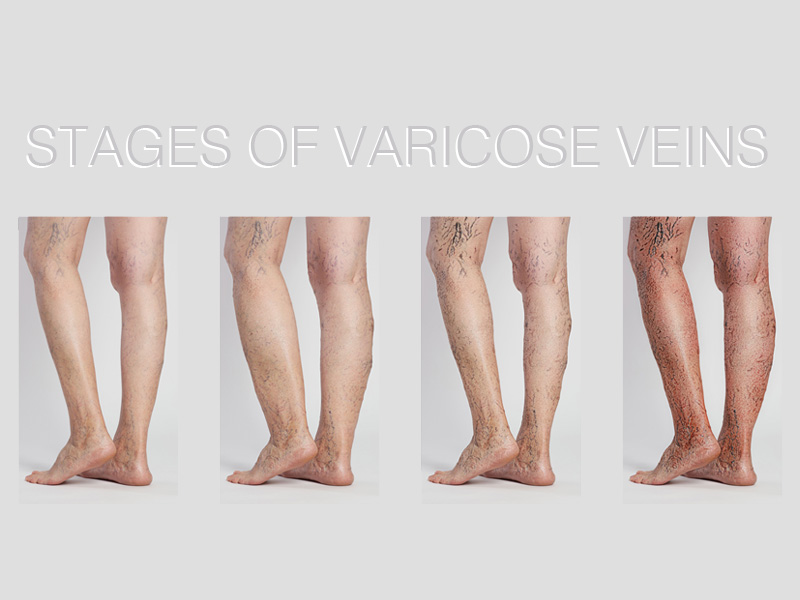
Varicose veins occur when the valves inside the veins that help direct blood back to the heart become weak or damaged. As a result, blood pools in the veins, causing them to swell and twist. Varicose veins are commonly found in the legs because they are farthest from the heart and subject to the effects of gravity.
Symptoms of varicose veins include:
- Swelling in the legs and ankles
- Heaviness or aching in the legs
- Throbbing or burning sensations around the veins
- Skin discoloration around the affected veins
- In severe cases, skin ulcers
What Is Cholesterol?
Cholesterol is a fatty substance found in your blood. Your body needs cholesterol to build healthy cells, but too much of it can lead to plaque buildup in your arteries, restricting blood flow. There are two types of cholesterol:
- LDL (Low-Density Lipoprotein): Known as “bad” cholesterol, LDL can lead to plaque buildup in the arteries.
- HDL (High-Density Lipoprotein): Known as “good” cholesterol, HDL helps remove excess cholesterol from the bloodstream.
Elevated levels of LDL cholesterol contribute to atherosclerosis, where arteries become narrow and hardened due to plaque buildup. This condition affects circulation and blood flow, increasing the risk of cardiovascular diseases such as heart attacks and strokes.
How Does Cholesterol Affect Varicose Veins?
While high cholesterol primarily affects the arteries, it can also indirectly impact venous circulation and worsen varicose vein symptoms. Let’s explore how cholesterol could aggravate varicose veins:
1. Poor Circulation and Blood Flow
Cholesterol-related arterial issues, such as atherosclerosis, can reduce overall blood flow and circulation. When cholesterol builds up in the arteries, it narrows and hardens them, limiting the flow of oxygen-rich blood. This condition can strain the veins, including those in the legs, forcing them to work harder to return blood to the heart.
Reduced circulation can lead to the following varicose vein-related issues:
- Increased blood pooling: Weakened circulation can cause blood to pool in the veins, worsening varicose vein symptoms such as swelling, heaviness, and pain.
- Delayed healing: Poor circulation also slows down the body’s ability to repair damaged vein walls, which may lead to more visible, bulging varicose veins.
2. Inflammation and Vein Damage
High cholesterol is often associated with chronic inflammation in the body. Plaque buildup in the arteries triggers an inflammatory response, which can damage blood vessels. This inflammation can also affect the veins, potentially worsening the structural integrity of the vein walls and increasing the risk of varicose veins.
How inflammation impacts varicose veins:
- Weakening of vein walls: Inflammation can further weaken the valves in the veins, which are already struggling to prevent blood from flowing backward. This can lead to worsening varicose veins.
- Increased discomfort: Inflammation is often accompanied by pain, which can intensify the throbbing, burning, and aching symptoms of varicose veins.
3. High Blood Pressure and Cholesterol
High cholesterol levels can contribute to elevated blood pressure, another risk factor for varicose veins. High blood pressure increases the force of blood against the vein walls, making it more difficult for veins to function properly.
The link between high blood pressure and varicose veins:
- Vein dilation: Over time, the pressure from high blood pressure can cause veins to stretch and dilate, making varicose veins more pronounced.
- Increased risk of complications: High blood pressure can increase the likelihood of developing serious complications from varicose veins, such as venous ulcers or deep vein thrombosis (DVT).
4. Obesity, Cholesterol, and Varicose Veins
There is a strong link between obesity, high cholesterol, and varicose veins. Being overweight or obese places extra pressure on the veins, particularly in the legs, making it harder for blood to flow back to the heart. This increases the likelihood of both varicose veins and high cholesterol, as poor diet and lack of exercise are common contributing factors to both conditions.
Obesity exacerbates varicose vein symptoms by:
- Adding pressure to the legs: Excess weight makes it harder for veins to pump blood, leading to worsened swelling, aching, and heaviness.
- Worsening cholesterol levels: Unhealthy eating habits associated with obesity can lead to higher LDL cholesterol levels, further impairing circulation.

Managing Varicose Veins and Cholesterol
To effectively manage both high cholesterol and varicose vein symptoms, consider these lifestyle changes:
1. Adopt a Heart-Healthy Diet
A diet that supports heart health is key to controlling cholesterol levels and reducing the strain on your veins. Focus on foods that promote good circulation and reduce inflammation.
Foods to include:
- High-fiber foods: Oats, whole grains, fruits, and vegetables help lower cholesterol and improve digestion.
- Healthy fats: Omega-3 fatty acids found in fish (salmon, mackerel), flaxseeds, and walnuts help reduce LDL cholesterol and promote healthy circulation.
- Antioxidant-rich foods: Berries, dark leafy greens, and green tea help fight inflammation and protect blood vessels.
2. Exercise Regularly
Physical activity helps improve circulation, lower cholesterol levels, and reduce blood pressure, all of which can benefit varicose vein symptoms.
Exercises to focus on:
- Walking: A simple but effective way to improve circulation in the legs and reduce varicose vein discomfort.
- Swimming: Low-impact exercise that promotes healthy circulation without putting extra pressure on the legs.
- Leg strengthening exercises: Calf raises, squats, and lunges can strengthen the muscles that support your veins.
3. Maintain a Healthy Weight
Losing excess weight helps reduce the pressure on your veins, improves circulation, and can lower cholesterol levels. Aim for gradual, sustainable weight loss through a combination of diet and exercise.
4. Quit Smoking
Smoking damages blood vessels and contributes to high cholesterol, worsening both varicose veins and cardiovascular health. Quitting smoking can improve circulation and reduce the risk of complications related to varicose veins.
5. Stay Hydrated
Proper hydration helps keep blood flowing smoothly and prevents it from thickening, which can lead to poor circulation. Drinking enough water throughout the day can alleviate varicose vein symptoms like swelling and discomfort.
6. Wear Compression Stockings
Compression stockings improve blood flow in the legs by applying gentle pressure, which can help reduce varicose vein symptoms such as swelling, heaviness, and aching.

FAQs About Cholesterol and Varicose Veins
1. Can high cholesterol cause varicose veins?
While high cholesterol does not directly cause varicose veins, it can worsen circulation and increase inflammation, which may aggravate existing varicose vein symptoms.
2. Can lowering cholesterol improve varicose veins?
Yes, lowering cholesterol levels can improve overall circulation, reduce inflammation, and potentially alleviate varicose vein symptoms like swelling and discomfort.
3. How does cholesterol affect circulation in varicose veins?
High cholesterol leads to plaque buildup in the arteries, reducing blood flow and placing extra strain on the veins. This can worsen varicose vein symptoms by increasing blood pooling and vein dilation.
4. What foods help lower cholesterol and reduce varicose vein symptoms?
Foods rich in fiber (oats, beans), healthy fats (fish, nuts), and antioxidants (berries, leafy greens) can help lower cholesterol and improve circulation, which may reduce varicose vein symptoms.
5. Can high blood pressure from cholesterol worsen varicose veins?
Yes, high blood pressure increases the force against vein walls, which can cause varicose veins to become more prominent and lead to complications like venous ulcers.
6. Is exercise important for managing cholesterol and varicose veins?
Regular exercise improves circulation, lowers cholesterol, and helps manage weight, all of which are important for reducing the symptoms of varicose veins.
A perfect Solution Of Varicose Veins Click Here



