Skin Discoloration and Ulcers: Are They Associated with Varicose Veins?
Varicose veins are a common vascular condition that affects millions of people worldwide. Most often seen in the legs, varicose veins occur when the valves inside the veins fail, causing blood to pool and veins to enlarge, twist, and become visible. While varicose veins are often viewed as a cosmetic issue, they can lead to more serious complications if left untreated. Two of the most significant and potentially harmful symptoms of advanced varicose veins are skin discoloration and ulcers.
These conditions are signs of chronic venous insufficiency (CVI), a long-term issue in which blood flow through the veins is severely impaired. In this article, we’ll explore how skin discoloration and ulcers are linked to varicose veins, why they develop, and what treatment options are available to manage these symptoms effectively.
Understanding Varicose Veins and Chronic Venous Insufficiency
Varicose veins develop when the one-way valves in the veins fail to function properly. Normally, these valves help push blood back to the heart against the force of gravity. When the valves become weak or damaged, blood flows backward and pools in the veins. Over time, this pooling of blood increases pressure within the veins, causing them to become enlarged, twisted, and visible just beneath the skin.
When varicose veins worsen or go untreated, the pressure inside the veins can affect surrounding tissues, leading to more severe symptoms like skin changes and ulceration. These symptoms are often linked to chronic venous insufficiency (CVI), a condition in which the veins struggle to pump blood effectively, leading to long-term complications.
How Does Skin Discoloration Develop in Varicose Veins?
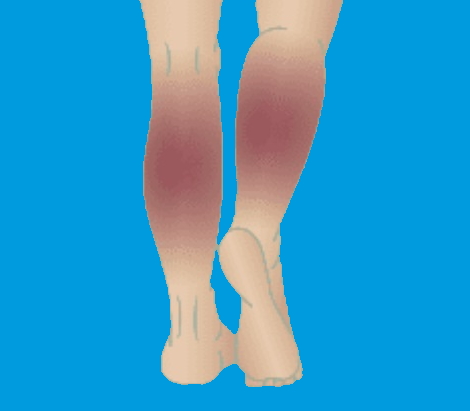
Skin discoloration is a common complication of varicose veins, particularly in advanced stages. This symptom occurs as a result of long-standing poor blood flow and increased pressure in the affected veins.
1. Hemosiderin Deposition and Hyperpigmentation
The most common form of skin discoloration in varicose veins is hyperpigmentation, where the skin becomes darker in the areas surrounding the affected veins. This discoloration often appears brown or reddish and is caused by the breakdown of red blood cells that have leaked out of the veins.
When blood pools in the veins, it can lead to small leaks of blood into the surrounding tissues. As the blood breaks down, it releases iron, which accumulates in the skin in the form of hemosiderin. This iron deposit causes the skin to darken, leading to brownish discoloration, particularly around the ankles and lower legs.
- Appearance: The skin may look patchy, brown, or reddish in color, and the discoloration often becomes more prominent over time.
- Location: Skin discoloration is typically seen around the ankles, but it can spread to other areas of the lower legs as varicose veins worsen.
2. Lipodermatosclerosis and Skin Hardening
In more advanced cases, chronic inflammation due to venous insufficiency can cause lipodermatosclerosis, a condition in which the skin becomes thickened, hardened, and sometimes painful. The chronic pooling of blood in the veins leads to inflammation in the surrounding tissues, and over time, the skin and underlying fat layer can become firm and discolored.
- Symptoms: Lipodermatosclerosis typically causes the skin to feel tight, shiny, and hardened. The skin may also appear reddish or brown due to the long-term buildup of hemosiderin.
3. Atrophie Blanche (White Scars)
Some people with severe varicose veins may develop small, white, scar-like patches on their skin, known as atrophie blanche. These white spots are areas of scarring that result from poor circulation and tissue damage. While they are not harmful on their own, atrophie blanche is often a sign of chronic venous insufficiency and may indicate a higher risk of ulcer formation.
How Do Ulcers Form in Varicose Veins?
Venous ulcers are one of the most severe complications of varicose veins and chronic venous insufficiency. They develop when the skin and underlying tissues break down due to prolonged pressure, poor circulation, and inflammation. Venous ulcers typically occur near the ankles and can be slow to heal, leading to discomfort and the risk of infection.
1. Causes of Venous Ulcers
Venous ulcers form when chronic inflammation and poor blood flow cause damage to the skin and underlying tissues. Over time, the pressure from pooled blood in the veins weakens the skin, making it more susceptible to injury. Even a small bump or scratch can result in an open sore that, due to the poor circulation in the area, struggles to heal.
- Poor oxygenation: The skin and tissues around varicose veins do not receive enough oxygen and nutrients, making it harder for wounds to heal.
- Venous hypertension: The increased pressure inside the veins pushes fluid into the tissues, leading to swelling, inflammation, and eventual tissue breakdown.
2. Symptoms of Venous Ulcers
Venous ulcers typically develop in the lower legs, just above the ankle. Early symptoms may include:
- Discolored skin around the ulcer, often brown or reddish
- Swelling around the affected area
- Pain or discomfort around the ulcer site, which may worsen with standing or walking
- Itching or irritation around the wound
As the ulcer develops, it appears as an open sore with a shallow base, and the surrounding skin may be inflamed or hardened. Venous ulcers can be quite painful and, if left untreated, may become infected.
3. Risk of Infection
One of the main concerns with venous ulcers is the risk of infection. Since ulcers are open wounds, they provide an entry point for bacteria, which can lead to cellulitis (a skin infection) or other serious complications. Signs of infection include increased pain, redness, swelling, and the presence of pus or an unpleasant odor.

Managing Skin Discoloration and Ulcers in Varicose Veins
Early intervention is key to preventing skin discoloration and ulcers from worsening. Several treatment options can help manage these symptoms and improve overall vein health.
1. Compression Therapy
Compression stockings are one of the most effective treatments for both skin discoloration and the prevention of ulcers. These stockings apply gentle pressure to the legs, improving blood flow and reducing the pooling of blood in the veins.
- Prevention of swelling and discoloration: By promoting better circulation, compression stockings can prevent fluid from leaking into the tissues, reducing the risk of skin discoloration and the formation of ulcers.
2. Wound Care for Ulcers
Proper wound care is essential for healing venous ulcers. This may include:
- Cleaning the wound: Regular cleaning of the ulcer with saline or a mild cleanser helps remove debris and prevent infection.
- Dressing changes: Special dressings, such as hydrocolloid or foam dressings, may be applied to protect the ulcer and promote healing.
- Debridement: In some cases, a healthcare provider may need to remove dead or damaged tissue to promote healing.
3. Medications and Topical Treatments
Anti-inflammatory medications or topical treatments, such as corticosteroid creams, can help reduce inflammation and relieve discomfort caused by skin discoloration and ulcers. Antibiotic creams may also be prescribed if there is a risk of infection.
4. Surgical or Minimally Invasive Treatments
For more severe cases of varicose veins, medical procedures such as sclerotherapy, endovenous laser therapy (EVLT), or vein stripping may be recommended to close or remove the damaged veins, improving blood flow and preventing further complications.
5. Lifestyle Changes
Making certain lifestyle adjustments can also help manage varicose veins and reduce the risk of developing skin discoloration and ulcers:
- Regular exercise: Walking or other forms of low-impact exercise can improve circulation and reduce the pressure in the veins.
- Elevating the legs: Elevating the legs when resting helps reduce swelling and improve blood flow back to the heart.
- Maintaining a healthy weight: Reducing excess weight can take pressure off the veins and prevent further damage.

Frequently Asked Questions (FAQs)
1. Can skin discoloration from varicose veins be reversed?
In the early stages, skin discoloration can be improved with treatments like compression therapy, lifestyle changes, and minimally invasive procedures. However, once discoloration becomes severe (due to hemosiderin deposition or lipodermatosclerosis), it may be more challenging to fully reverse.
2. Are venous ulcers dangerous?
Yes, venous ulcers can be dangerous if left untreated. They are at risk of becoming infected, which can lead to more serious complications. Prompt treatment and proper wound care are essential.
3. What is the best treatment for venous ulcers?
The best treatment for venous ulcers includes compression therapy, proper wound care, and, in some cases, minimally invasive procedures to improve circulation. Infected ulcers may also require antibiotics.
4. How can I prevent skin discoloration from varicose veins?
To prevent skin discoloration, focus on improving circulation through regular exercise, wearing compression stockings, elevating your legs, and avoiding long periods of standing or sitting.
5. What causes ulcers to form in varicose veins?
Ulcers form due to long-standing venous insufficiency, where poor circulation and increased pressure in the veins cause the skin and tissues to break down.
6. When should I see a doctor about skin discoloration or ulcers?
You should see a doctor if you notice persistent skin discoloration around varicose veins, swelling, or if you develop an open sore (ulcer) that does not heal within a few days or shows signs of infection.
A perfect Solution Of Varicose Veins Click Here



